Now more than ever, hospitals are leaning on state-of-the-art software to make the work they do every day more accurate and more efficient. The right software can improve patient experience and treatment quality while dramatically saving hospitals time and money.
In this guide, we’ll explain how Eon’s lung cancer screening software helps you do more with your EHR. Plus, we’ll walk through our recommended review methods and integration advice.
The Review Committee
Purchasing and implementing an organization-wide software can affect a lot of different areas of your hospital. That’s why it’s important to establish a diverse review committee representing a range of departments. Here are a few things for your review committee to consider when evaluating any software solution:
Domain Expertise
Look for a solution designed by providers, not engineers. Providers understand provider workflows and clinical pathways, and know how to minimize data entry and optimize the effort of the staff. Ultimately, a well-designed application should adjust to your workflow—not the other way around.
Experience
When choosing a software provider, look for someone who has executed in multiple environments, including integrating with multiple EHR’s in complex environments. The right partner will provide resources from every customer, not just one or two hand-picked customers.
Vision
Look for a company that is agile. This means understanding where the market is going and how to be a good vendor partner to meet your unique environment’s needs.
Solutions
Today’s needs are one thing, tomorrow’s needs are another. When choosing a partner, look for a company who can iterate quickly and meet the future needs of healthcare providers. Avoid “orphan apps” that don’t address multiple disease states.
Price
Why pay for a large company’s overhead costs when technology is increasingly becoming cheaper and easier to build? Look for a company that will have a cost ceiling and not upcharge you every chance they get.
What to look for in patient management and lung cancer screening software
Cloud based
Cloud-based software solutions increase efficiency and flexibility, while dramatically reducing cost. With Eon’s cloud-based software, there are zero upgrade fees, no infrastructure costs, endless scalability, and automation for otherwise laborious tasks.
Patient Registration
Traditional registries can come with silos and barriers. This makes registration difficult, especially when your patients source from many different locations and systems. By allowing registration to span different environments, Eon creates increased flexibility and makes it easier than ever to increase patient volume over time.
Longitudinal Tracking
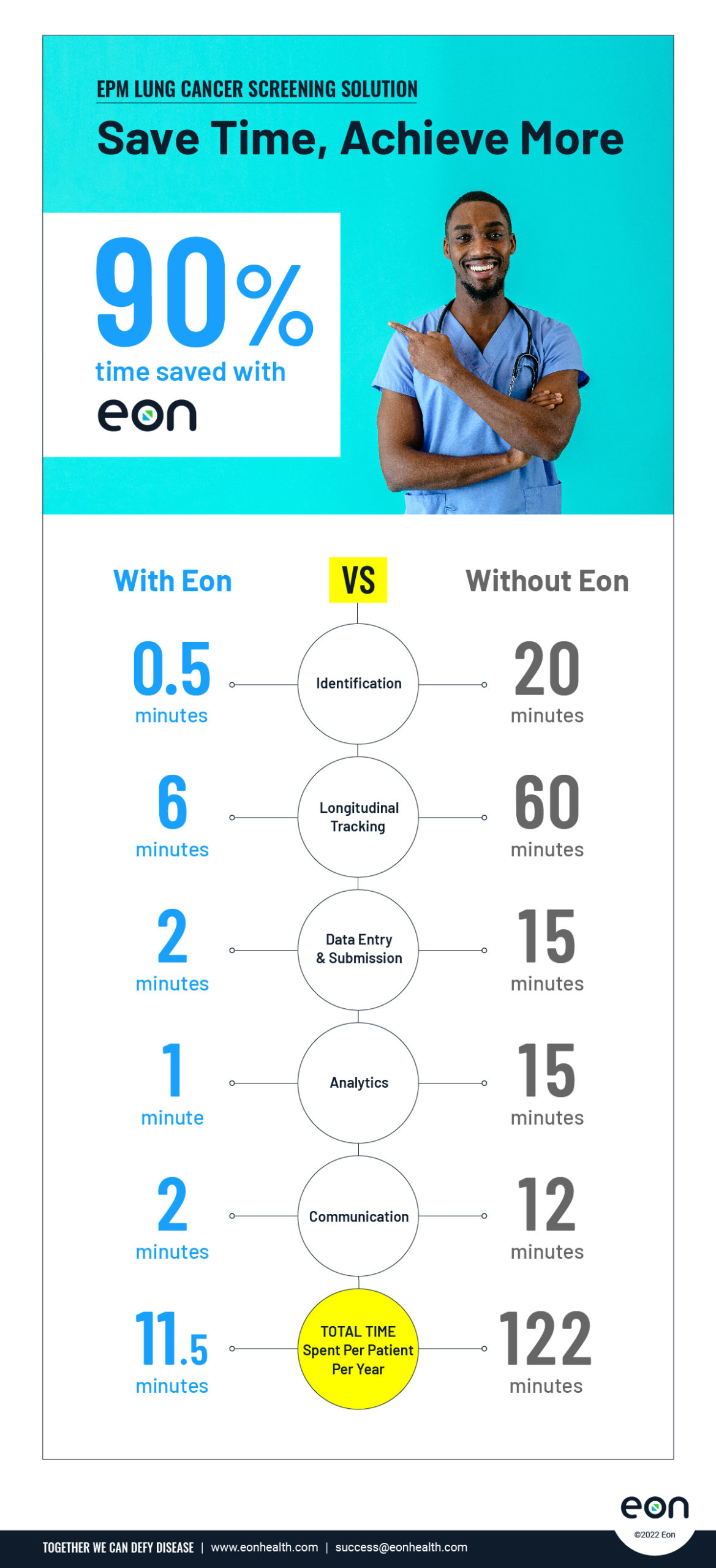
Workflows should be adaptable to your environment. That’s why Eon’s lung cancer screening software uses Robotic Process Automation (RPA) to automate repetitive lung cancer screening tasks so all of your expected procedures and exams are automatically populated. That means 90% of your patients’ next expected exams are already there, so you instantly know what’s already been scheduled and what needs to be scheduled. This enables FTEs to spend more time on at-risk patients and value-added tasks that drive downstream revenue.
Follow-up Listener
Eon also lets you know what patients actually received their exams or procedures, and which ones are at risk for being lost to follow-up. Eon’s proprietary Follow-Up Listener technology listens for expected exams to become scheduled in EPM and matches pertinent performed exams to scheduled exams. The software also predicts patient no-shows and creates patient leakage information, enabling hospitals to make strategic interventions if necessary.
AI Technology
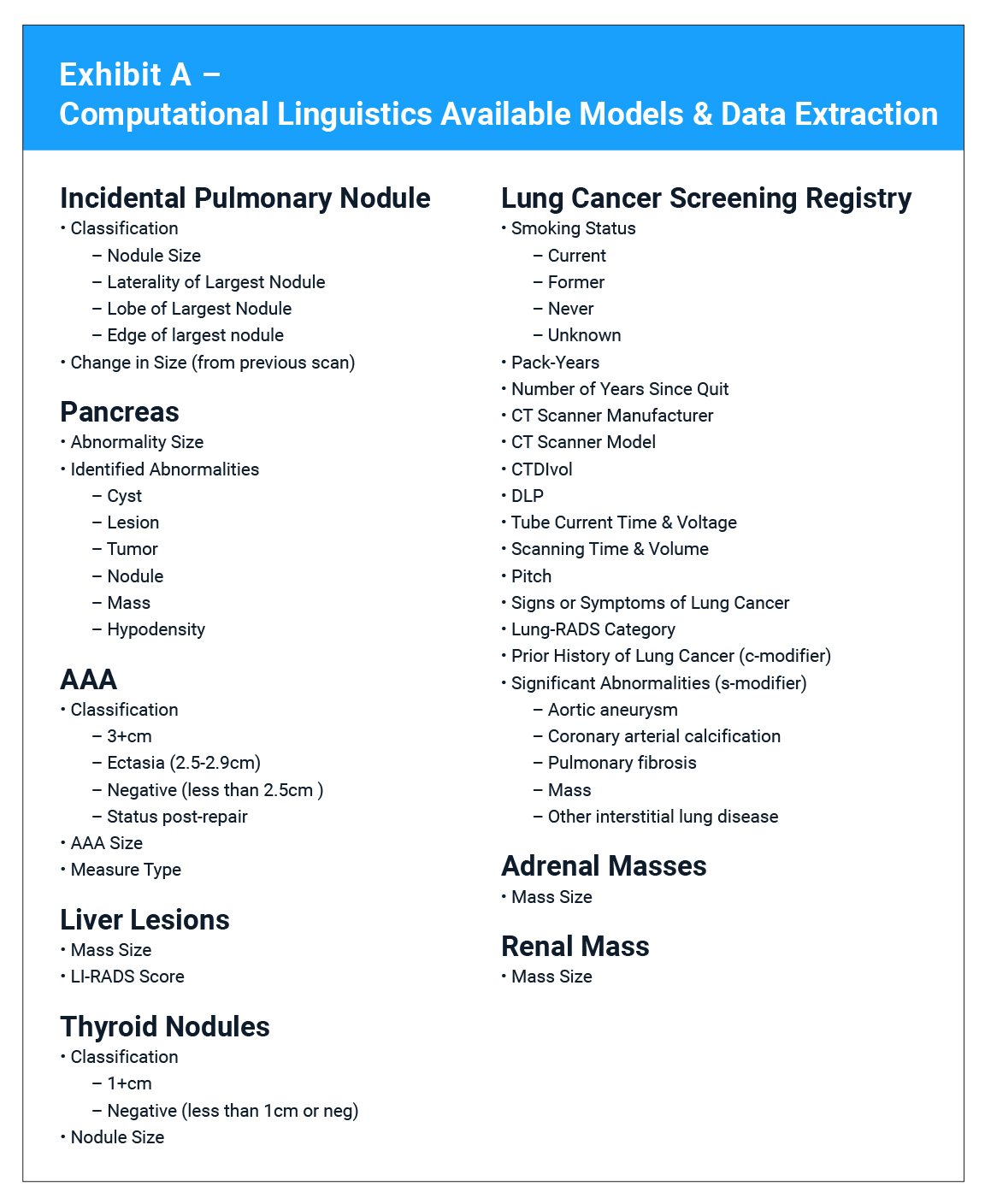
Technologies like Computer Aided Detection (CAD) and Natural Language Processing (NLP) can disrupt radiology workflow. Eon uses the most advanced form of AI to create layered Computational Linguistics (CL) data science models. CL understands text and the linguistic structure of English, similar to how the human brain reads, eliminating the need to require any changes to radiology workflow. This approach helps Eon achieve 98.95% accuracy and 98.66% recall—reducing the number of false positives while increasing patient retention. In addition, Eon’s software identifies incidental pulmonary nodules at a rate ten times greater than standard identification methods.
Zero Data Entry
Eon’s lung cancer screening software makes data entry easier than ever by allowing you to enhance, refine, and improve raw data with a robust data-enrichment toolset. Our computer models are integrated with traditional data engines, allowing for never-before-seen patient data automation. Plus, with Eon’s ACR submission software, you get real-time flags on required data fields for LCSR submission, CMD, NRDR, IELCAP, or research and clinical trial requirements—so you never have to guess if you’re in compliance.
Real-time Analytics
It’s crucial to be able to see a clear, concise overview of your key results from lung cancer screening, incidental nodule tracking, and clinical trial activity in order to track trends and measure growth. But overviews aren’t enough. With complex patient management data, it’s important to create visualizations in order to bring your data to life. With Eon’s state-of-the-art analytics tools, you can create and export custom reports that help you analyze and visualize your results more easily than ever. Plus, Eon’s lung cancer screening software takes the busywork out of incidental nodule tracking by allowing you to assign data fields to specific users and get access to all required data fields—with just one click.
One Click LCSR Submission
With Eon’s ACR submission software, you can automatically audit and submit to the National Radiology Data Registry, RedCap, and other clinical trial registries with one click. Plus, the software includes NRDR confirmation of accepted data—you never have to guess if your CMS-required LCSR submission was accepted.
Patient and Provider Communication
Eon’s communication portal lets you automate, document, and track all of your communication, all in one place. You can create custom letters with automated content associated with a specific patient and their specific results, organized in a way that makes sense to you. Then you can send, fax, batch, print or email with a single click.
Implementation Expectation
There’s a lot that goes into carefully selecting the software that will best fit the current and future needs of your hospital. But that’s not all you need to consider. Ensuring a quick and seamless implementation of the software is crucial in realizing a return on your investment as quickly as possible. That’s why the topic of implementation must be a part of any vendor evaluation. Here are a few things we recommend considering:
Proven
Consider each vendor’s implementation experience. Specifically, ask vendors to provide references for their fastest implementation and their longest implementation. You don’t need a vendor to learn on your dime. Choose a vendor that is proven and experienced.
Solution-Oriented
Do vendors rely heavily on your IT team to create solutions? Or, are they experienced and able to provide solutions for you without dragging in additional resources?
No more than 8 weeks
No one wants to wait. While each implementation scenario may be unique, 8 weeks or less should be the standard for technical implementation of any organizational-wide software. This ensures that you start realizing a return on your investment as quickly as possible. Eon offers a 7-day implementation of its lung cancer screening software.
Do more with your EHR, with Eon.
Eon provides complex patient management software for today’s hospital. We believe data is the lifeblood of healthcare. That’s why we’re using state-of-the-art technology to revolutionize everything from incidental nodule tracking and complex LCSR submissions to patient communication and follow-up.